 Image 1 of 8
Image 1 of 8

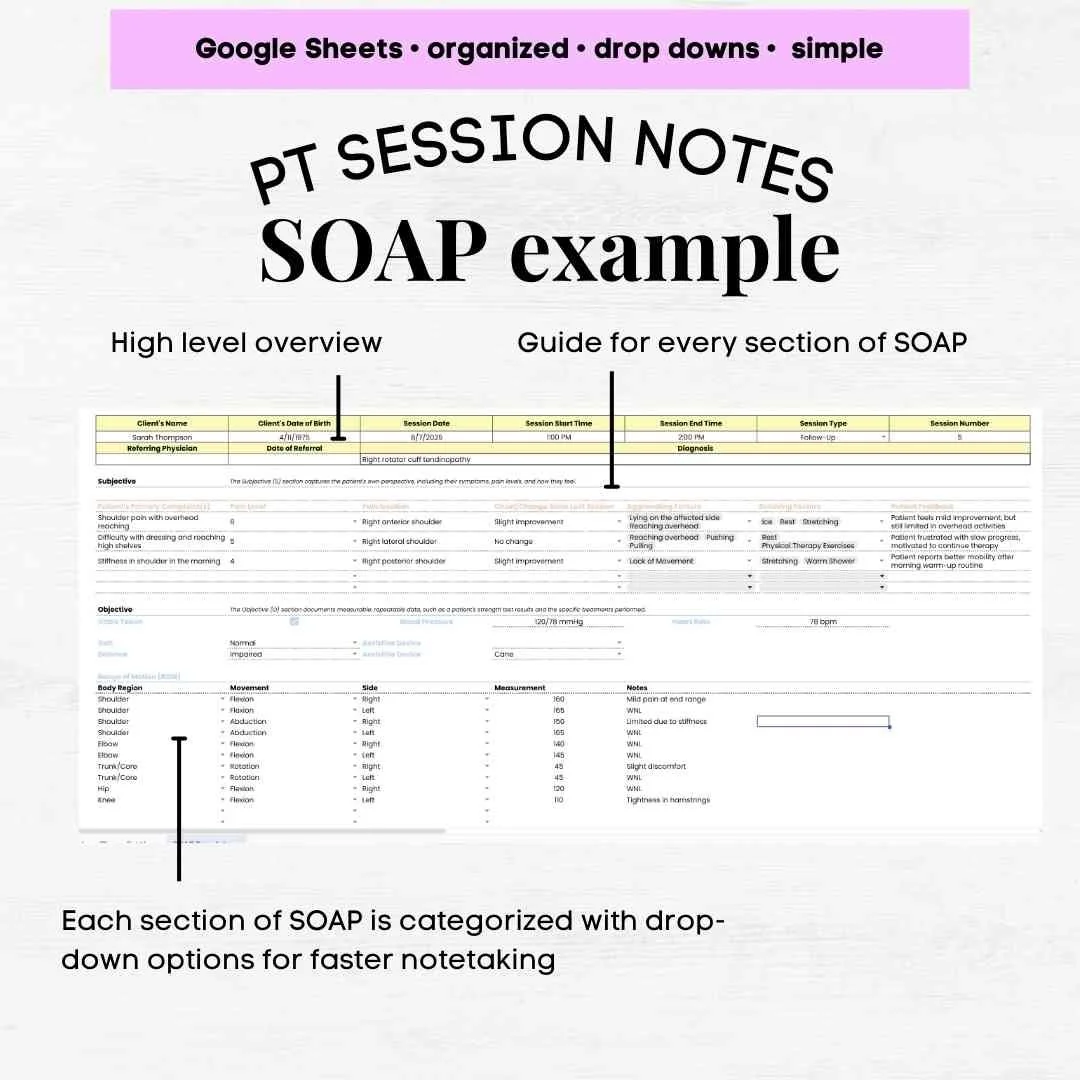 Image 2 of 8
Image 2 of 8
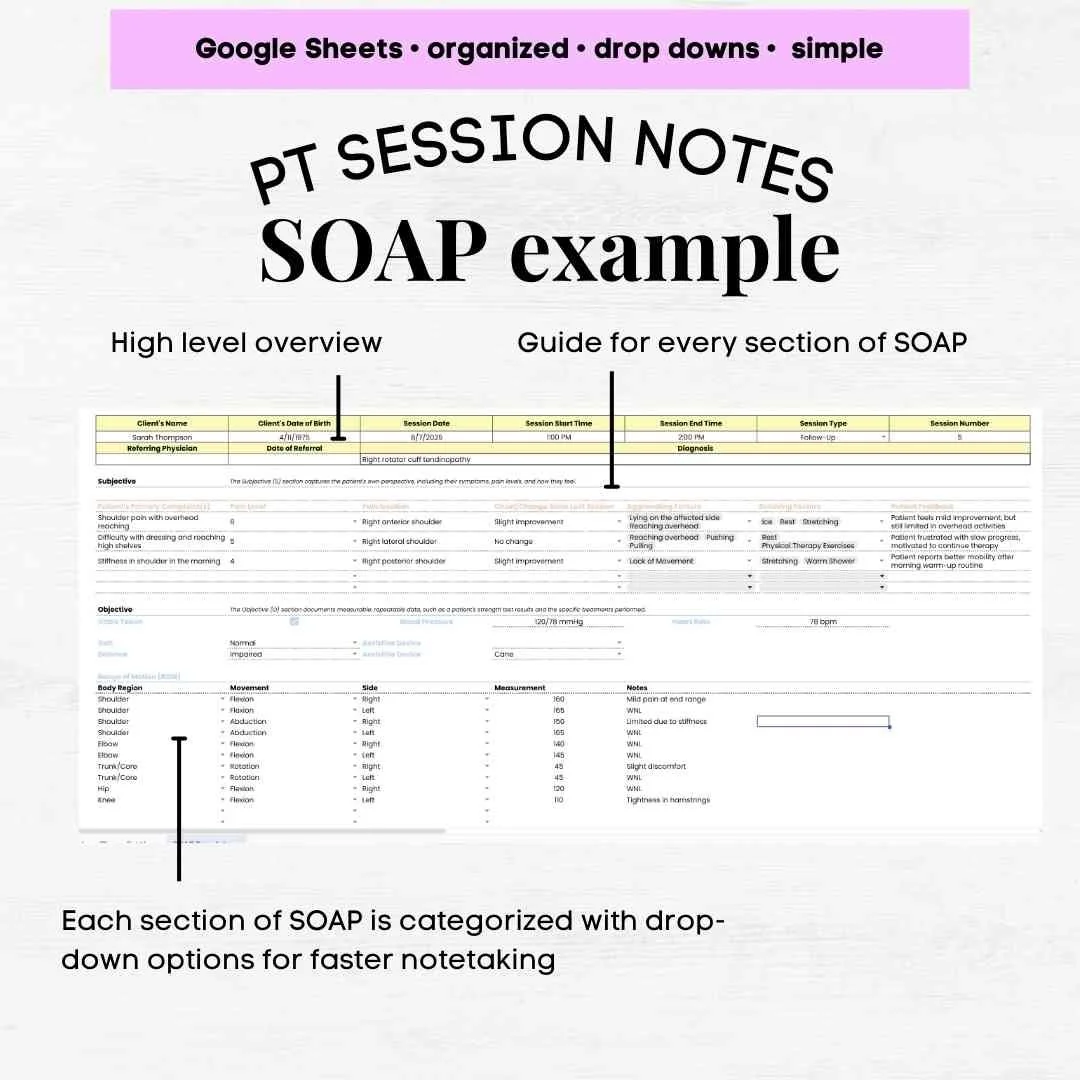
 Image 3 of 8
Image 3 of 8

 Image 4 of 8
Image 4 of 8

 Image 5 of 8
Image 5 of 8

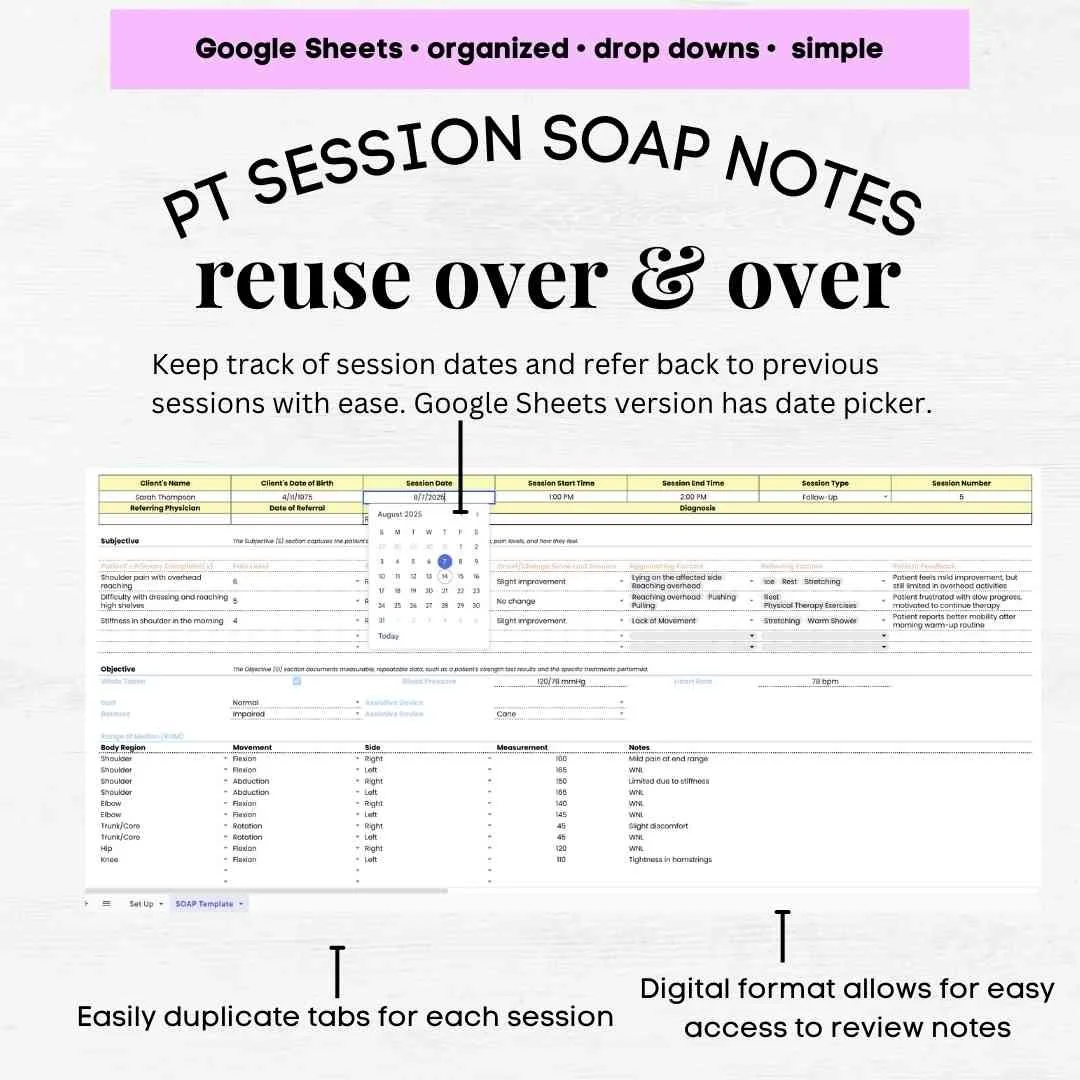 Image 6 of 8
Image 6 of 8
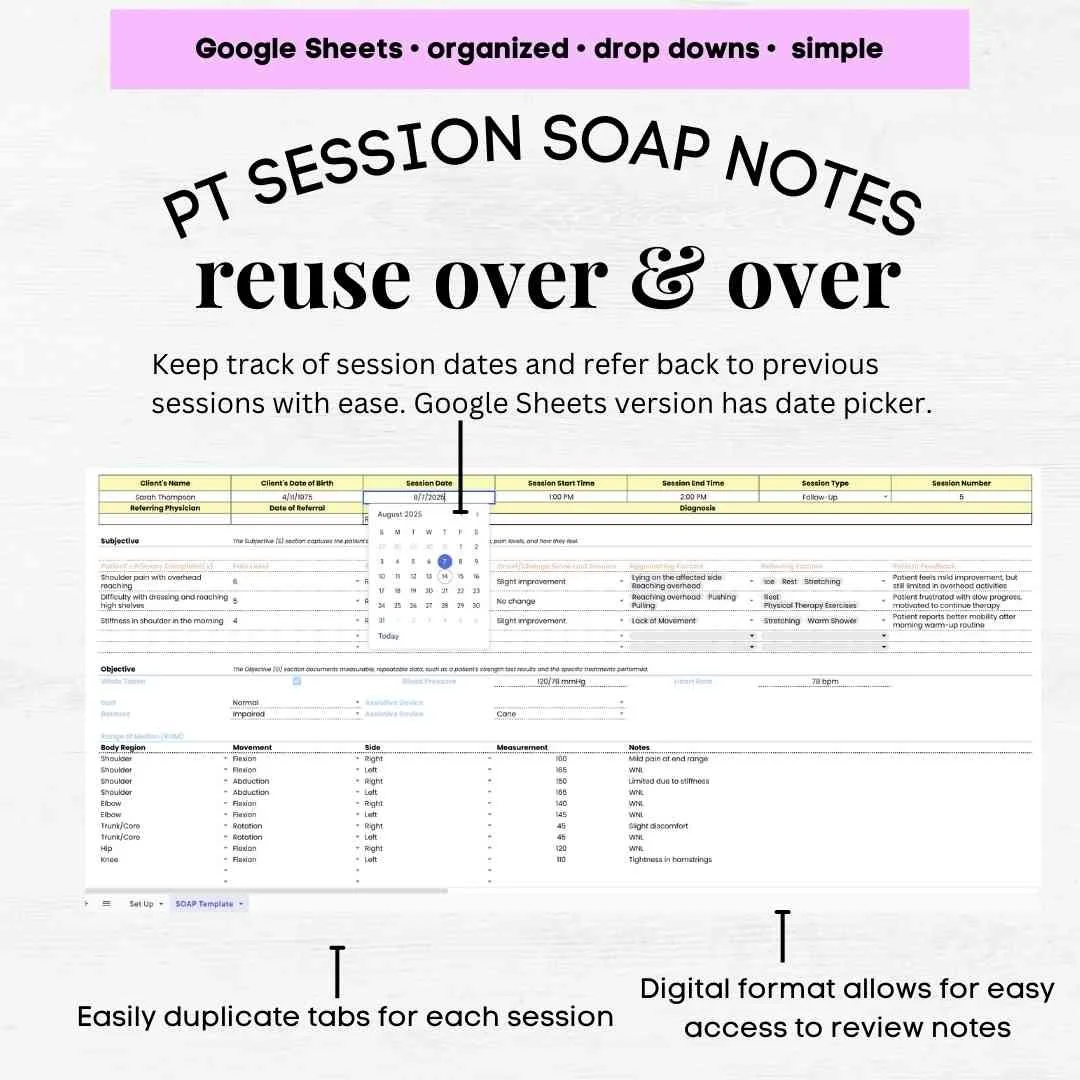
 Image 7 of 8
Image 7 of 8

 Image 8 of 8
Image 8 of 8


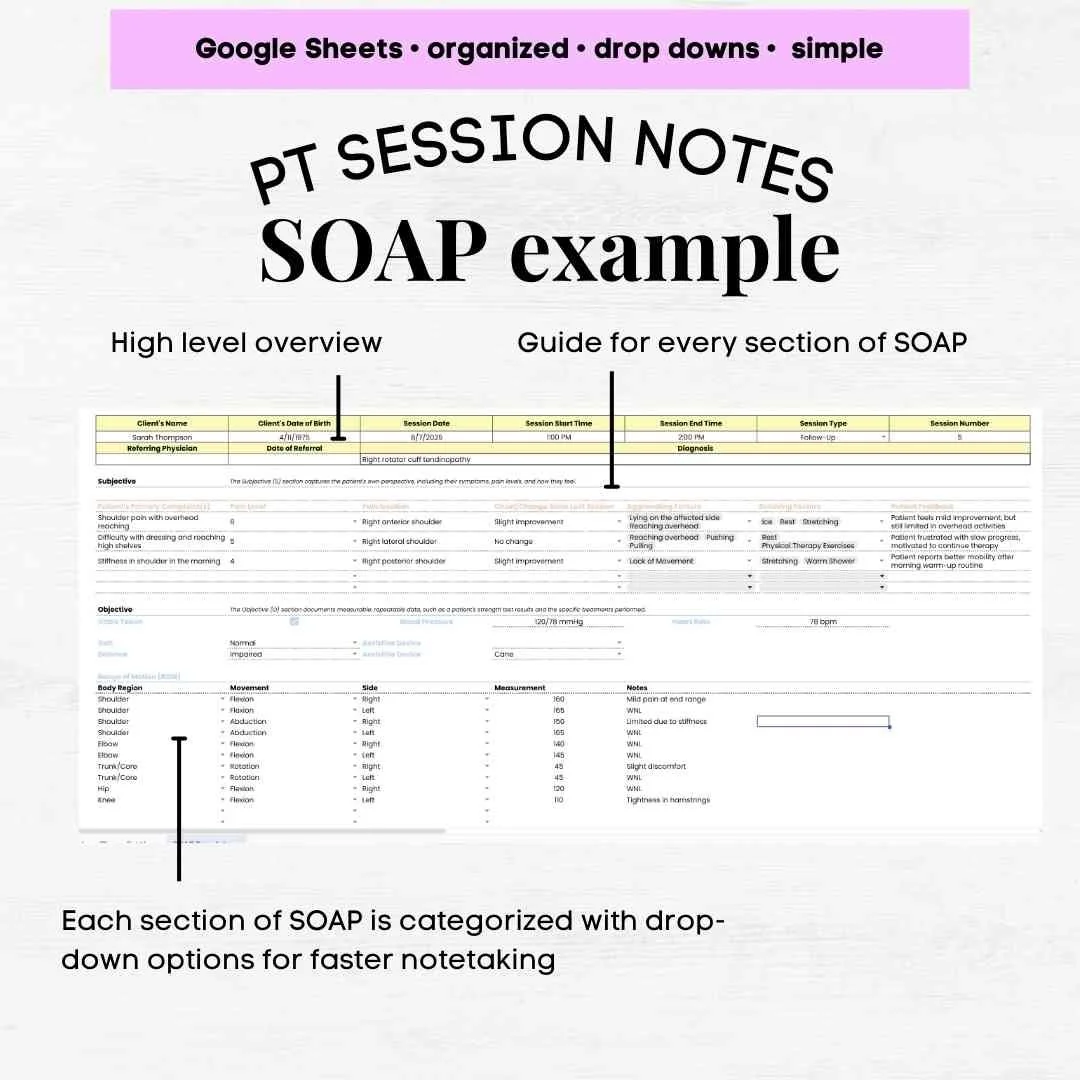



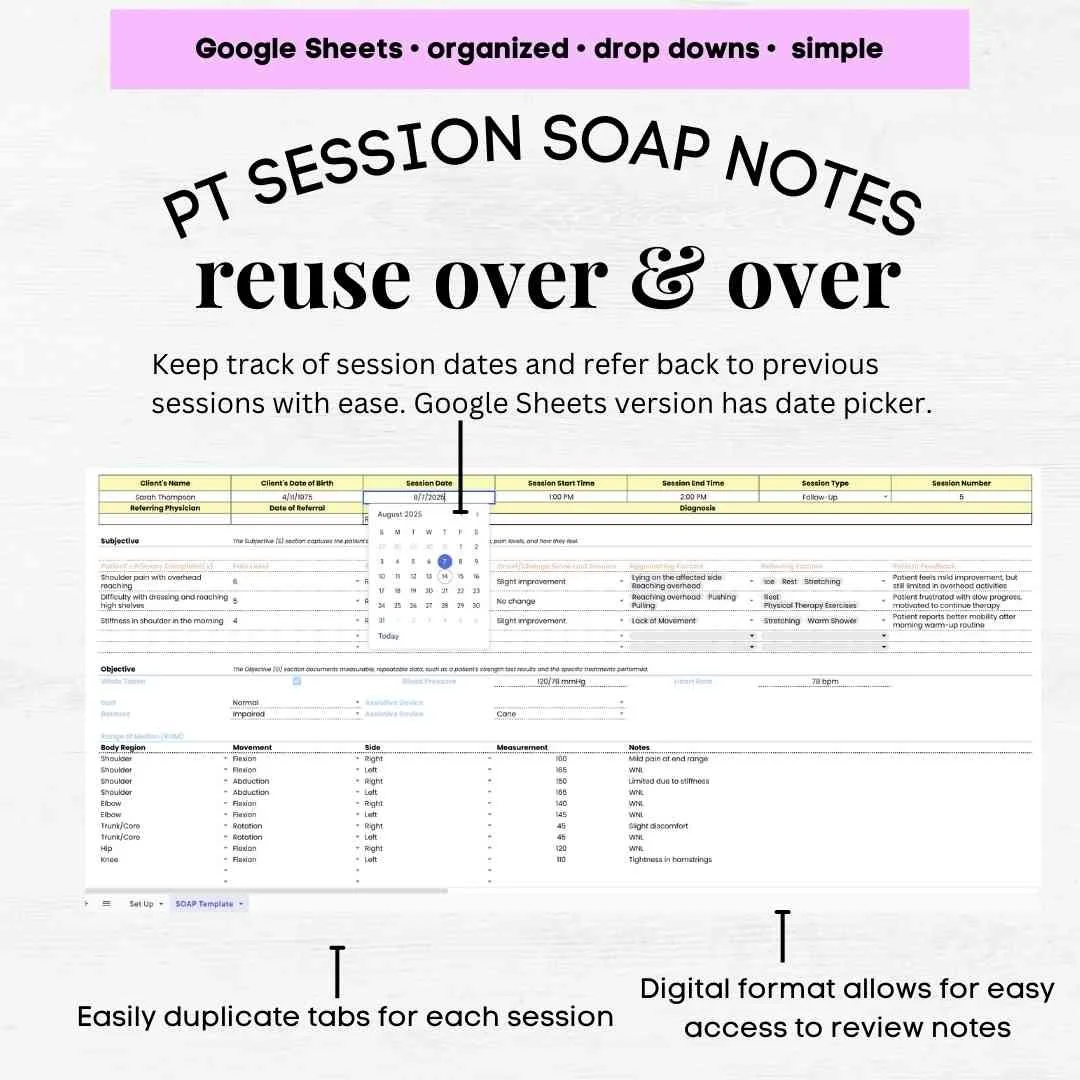


Physical Therapy SOAP Note Template
Physical Therapy SOAP Note Template – PT SOAP Note Example & Assessment Guide
Streamline your documentation process with this Physical Therapy SOAP Note Template—perfect for PTs, DPTs, and rehab professionals. Designed for clarity and compliance, this easy-to-use template helps you quickly capture patient information, progress, and treatment details while maintaining professional standards.
This template includes a PT SOAP Note Example to guide you in writing accurate and concise notes, plus a PT SOAP Note Assessment Example so you can document evaluations confidently. Whether you’re a student learning documentation skills or a seasoned therapist looking to save time, this tool ensures you cover all PT SOAP Note sections—Subjective, Objective, Assessment, and Plan—without missing critical details.
This template includes everything you need for thorough patient documentation:
Subjective: Patient-reported symptoms, pain scale, progress updates, and functional limitations
Objective: Detailed clinical findings including range of motion (ROM), strength testing, flexibility, balance, posture, gait, neurological testing, and special test results
Assessment: Clinical impressions, PT SOAP note assessment example fields, progress toward goals, and changes in treatment plan
Plan: Next steps, updated goals, therapeutic interventions, frequency/duration, and home exercise programs
Features:
Editable, ready-to-use PT SOAP Note Template
Clear PT SOAP Note Assessment section for streamlined evaluations
Professional PT SOAP Note Example for guidance
Printable and digital-friendly formats
Ideal for physical therapy, sports rehab, and home health care
Write professional notes faster, improve documentation accuracy, and keep your patient records organized with this Physical Therapy SOAP Note Template—your go-to reference for efficient and compliant PT documentation.
Physical Therapy SOAP Note Template – PT SOAP Note Example & Assessment Guide
Streamline your documentation process with this Physical Therapy SOAP Note Template—perfect for PTs, DPTs, and rehab professionals. Designed for clarity and compliance, this easy-to-use template helps you quickly capture patient information, progress, and treatment details while maintaining professional standards.
This template includes a PT SOAP Note Example to guide you in writing accurate and concise notes, plus a PT SOAP Note Assessment Example so you can document evaluations confidently. Whether you’re a student learning documentation skills or a seasoned therapist looking to save time, this tool ensures you cover all PT SOAP Note sections—Subjective, Objective, Assessment, and Plan—without missing critical details.
This template includes everything you need for thorough patient documentation:
Subjective: Patient-reported symptoms, pain scale, progress updates, and functional limitations
Objective: Detailed clinical findings including range of motion (ROM), strength testing, flexibility, balance, posture, gait, neurological testing, and special test results
Assessment: Clinical impressions, PT SOAP note assessment example fields, progress toward goals, and changes in treatment plan
Plan: Next steps, updated goals, therapeutic interventions, frequency/duration, and home exercise programs
Features:
Editable, ready-to-use PT SOAP Note Template
Clear PT SOAP Note Assessment section for streamlined evaluations
Professional PT SOAP Note Example for guidance
Printable and digital-friendly formats
Ideal for physical therapy, sports rehab, and home health care
Write professional notes faster, improve documentation accuracy, and keep your patient records organized with this Physical Therapy SOAP Note Template—your go-to reference for efficient and compliant PT documentation.
